Patient Volume: Trends and Threats
How do hospitals stay in business? One of the most prevalent revenue drivers for hospitals is patient volume. Without patients to care for, hospitals quickly become an abyss of expenses that lead to a negative bottom line. When the pandemic hit in 2020, hospitals and health systems around the country questioned whether they could stay afloat. The vast majority of their resources were devoted to caring for patients with COVID-19, while more profitable service lines were curtailed due to capacity constraints and declining demand for elective services. More than 36 hospitals entered bankruptcy during 2020, and financial losses for hospitals and health systems were projected to reach at least $323.1 billion by the end of that year.[i] The situation might have been even worse without funding made available to many hospitals through federal COVID relief programs such as the Provider Relief Fund.
Naturally, patient volumes slowly began to re-emerge after the initial waves of COVID settled; however, hospitals hopeful for the return of normal patient volumes experienced a sharp shift in where that returning volume landed. Some services historically provided in inpatient settings began moving to outpatient locations, and outpatient services began moving out of the hospital entirely to lower-acuity settings such as Ambulatory Surgery Centers (ASCs). Revenue is only one part of the equation; expenses play an important role in the determination of net income as well. Hospitals and health systems are under a great deal of pressure to increase patient volume with the goal of raising revenue, while also decreasing expenses to generate income. The disaggregation of volume moving into lower acuity settings places hospitals is a push-pull situation. Lower acuity settings are typically lower-cost settings, which means hospitals can decrease overall costs if they shift services to an outpatient center or ASC. However, lower acuity settings also translate to lower reimbursem*nt rates. Both payers and patients are driving the shift in place of service, though perhaps for different reasons. Governmental and commercial payers are the most significant source of revenue for healthcare entities and dictate the majority of revenue a hospital may generate from a particular service. These payers prefer to push volume toward lower-acuity settings when clinically appropriate because they are able to pay less for the same service. On the other side, patients may prefer an outpatient setting or ASC because the services are more affordable and often more convenient. While hospitals and health systems have slowly recovered from the low-volume years of COVID, the post-pandemic era has forced these entities to be much more intentional in managing their profit margins.
Site-Neutrality
Hospitals have already been battling the shift in volume away from the inpatient setting, but that is not the only challenge they face. Several proposals seek to expand “site-neutral” reimbursem*nt. This approach determines the reimbursem*nt amount based on the setting where a particular service is most frequently performed, regardless of where the actual procedure occurs. Knee surgeries, for example, can be performed in both hospital outpatient and ASC settings. Proposals for site-neutral payments dictate that while services may still be performed in either type of facility, they would be reimbursed at the rate related to the setting where that service is performed most frequently. Said another way, if a service is most frequently performed in a physician office setting, the reimbursem*nt amount would reflect the physician office rate even if the procedure is performed at an ASC or hospital. In ascending order, physician offices typically receive the lowest reimbursem*nt rate of all sites of service due to lower overhead costs. ASCs are next in line, followed by hospital outpatient settings, with hospital inpatient settings receiving the highest reimbursem*nt for services. Accordingly, the proposed site-neutrality rules have the potential to decrease hospital revenue even further.
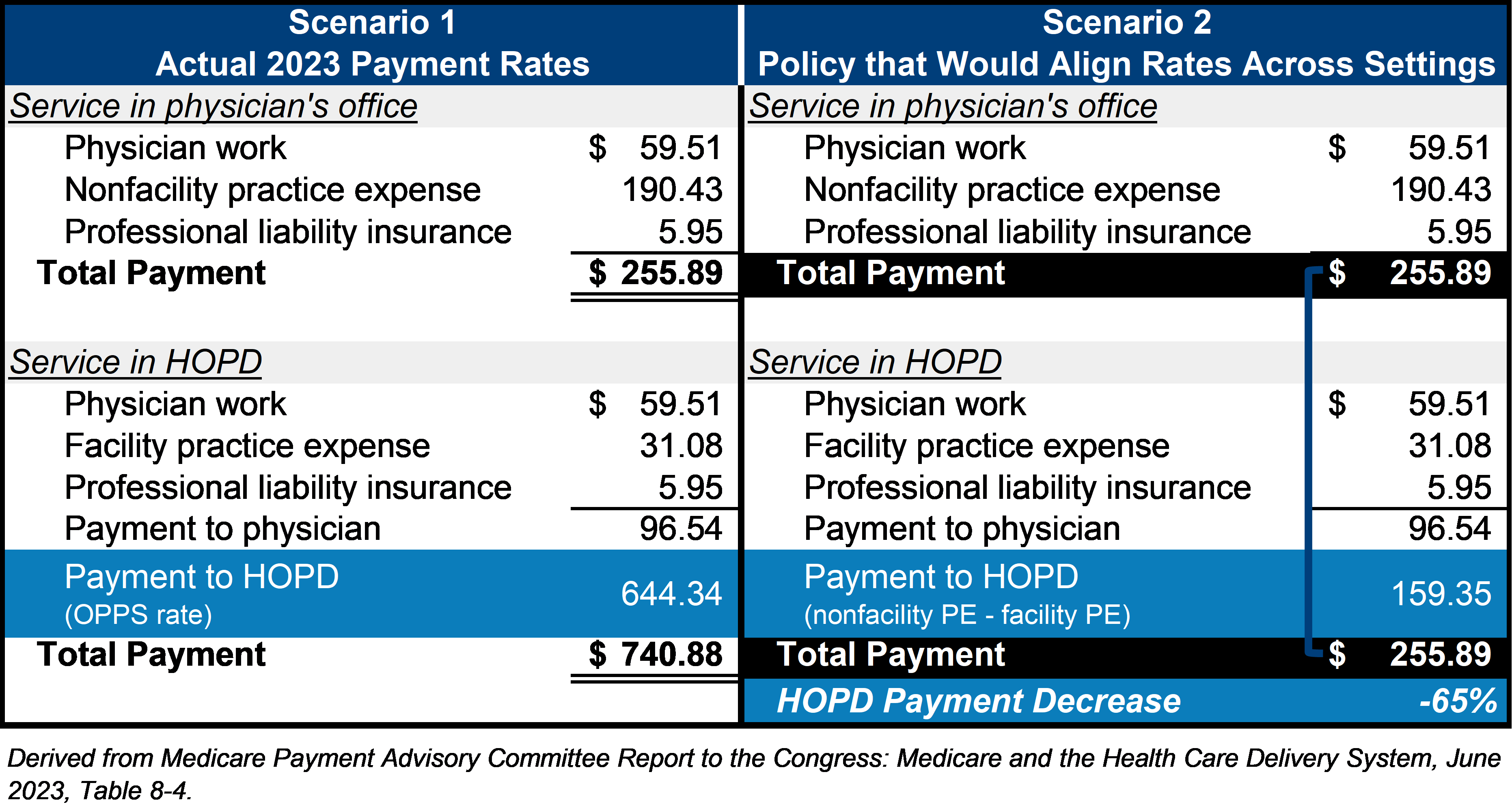
Under the Medicare Physician Fee Schedule, the portion of reimbursem*nt related to physician work and professional liability insurance is the same regardless of where a service is performed. The only difference relates to the practice expense (PE) component of reimbursem*nt. If the service is provided in a freestanding office, the physician receives additional reimbursem*nt, known as the nonfacility PE, to cover the overhead (office building, equipment, clinical staff, medical supplies, etc.). If the service is instead provided in an ASC or a hospital outpatient department (HOPD), the physician receives a lower amount, the facility PE, to cover expenses associated with the procedure, while the facility in which the procedure was performed receives an additional payment under what is called the outpatient prospective payment system (OPPS). Again, this payment is intended to cover the direct and indirect expenses associated with rendering the service at that location.
In 2023, the Medicare Payment Advisory Commission (MedPAC) recommended that Medicare fee-for service payment rates should be aligned across ambulatory settings based on “the resources needed to treat patients in the most efficient setting” where the service can be “safely and appropriately provided.”[ii] To illustrate the potential impact of site-neutrality provisions, the chart below details the various components of reimbursem*nt for a lumbar epidural injection under a methodology proposed by MedPAC[iii]. Under Scenario 2, the reimbursem*nt rate for the service provided in an HOPD is adjusted down to reflect the difference between the nonfacility PE ($190.43) and the facility PE ($31.08). This results in a total payment equivalent to the reimbursem*nt had the service been rendered in the physician’s office – a 65% decrease from the previous HOPD payment rate. Of course, this difference would be magnified by the volume of procedures that would take a reimbursem*nt hit.
Legislative proposals that have been introduced include the following, with each containing site-neutrality provisions that would be implemented beginning in 2025:
The PATIENT Act of 2023 (H.R. 3561) and the Lower Costs, More Transparency Act (H.R. 5378) – According to the American Hospital Association (AHA), both of these bills would apply site-neutrality reductions to reimbursem*nt for drug administration services provided in off-campus HOPDs that are currently grandfathered from such policies. AHA estimates that this would result in a $4.1 billion reduction in reimbursem*nt over a 10-year period.[iv] The Lower Costs, More Transparency Act was passed by the House of Representatives in December 2023.
Site-based Invoicing and Transparency Enhancement (SITE) Act (S. 1869) – According to AHA, this legislation would also result in site-neutral payment cuts in grandfathered off-campus HOPDs but would extend the policies to all services provided at such locations (except for office evaluation and management visits, which are already subject to site neutrality.) This would have a significant impact, estimated to be as much as $34.3 billion over 10 years.[v]
Medicare Patient Access to Cancer Treatment (MPACT) Act (H.R. 4473) – This is a narrower proposal that would adopt site-neutrality at off-campus HOPDs in connection with certain cancer treatment, with an estimated 10-year impact of $11.8 billion.[vi]
These proposals clearly pose yet another threat to hospital margins and would have a significant negative financial impact on hospitals. As long as volume moves toward ASCs and physician offices, reimbursem*nt rates and therefore revenue for hospitals is decreasing, even if the volume simply moves from the inpatient to the outpatient setting within a health system. This leaves hospitals less revenue to cover the costs of operating a 24/7 facility, including building and equipment costs, specialty services that are required to be available regardless of patient volume, clinical support staff, and more. Historically, many of the elective services that are now shifting to outpatient settings have been highly profitable, with such profits subsidizing some of the lower margin inpatient services. Therefore, hospitals will need to find other revenue sources to bridge that gap.
Creativity to Manage the Margin
Given the risks stemming from site-neutrality proposals and the continuing trend of services moving toward lower-acuity settings, hospitals and health systems will need to exercise creativity to maintain their profit margins. In the past, a common strategy was to negotiate for higher rates with commercial payers; however, payers are also actively trying to rein in costs, making higher rates far from guaranteed. Further, commercial payers typically follow Medicare in reimbursem*nt models and these payers will likely adopt their own site-neutral reimbursem*nt policies over time. Revenue cycle improvement, creative joint-ventures, expansion of sites of care, and improved operating efficiencies will all need to be a part of the mix to stabilize margins.
The bottom line is that there will always be emergent cases and high-acuity care that must be – and can only be – provided in the hospital, and access to such care must be preserved. Hospitals can provide trauma and inpatient services that no other healthcare settings can offer, yet the decline in overall hospital revenue could put high-acuity care in jeopardy. Hospitals are expensive to operate, and expenses will be a significant factor when considering how to maintain sustainable margins. This may mean assessing underperforming service lines and making difficult decisions about whether certain services should be discontinued. Hospitals may also consider acquiring or building an ASC, which would preserve revenue within the organization rather than lose it to independent facilities. It may also benefit rural and community hospitals to become a part of larger health systems to ensure adequate leverage with payers.
There are clearly many factors at play as it relates to managing hospital profit margins, and it may not be as simple as cutting expenses or generating more revenue. As the healthcare environment continues to evolve, entities that provide patient care must adapt to the trends of their industry if they are to thrive and meet the needs of patients in their communities.
JTaylor recognizes that these site-neutral reimbursem*nt proposals could have a material impact on hospital outpatient operations, in particular. Our team of experienced professionals can help assess this potential impact by analyzing utilization trends and applying reimbursem*nt assumption. Further, we can help you develop a robust operational strategy, explore joint venture opportunities, or determine whether additional state or federal programs might be available.
Herd A. Midkiff, CVA
Partner – Consulting Services
817.546.7036 | [email protected]
Herd has over 20 years of experience serving clients in the healthcare, non-profit, and investor-owned sectors. He has extensive experience in strategic planning, including joint ventures, business acquisition, due diligence services, and managed care contracting support. He also draws upon his healthcare and finance background to provide business enterprise and compensation valuation services. His clients include large multi-hospital health systems, physician-owned hospitals, entrepreneurs, and attorneys.
Kyle W. Kirkpatrick, FACHE
Partner – Director of Consulting Services
214.675.3608 | [email protected]
Kyle has over 25 years of consulting and operational experience working in healthcare and life sciences with public and private organizations across the nation. He is a former hospital CEO with experience running hospital groups, managing joint ventures, implementing new strategies, driving EBITDA enhancements, and creating positive organizational cultures. He has worked as a consultant within Big 4 firms focused on strategic planning, M&A, and operational improvements.
[i] American Hospital Association. (2020, November). Fact Sheet: COVID-19 Pandemic Results in Bankruptcies or Closures for Some Hospitals. https://www.aha.org/system/files/media/file/2020/11/fact-sheet-covid-hospital-bankruptcies-1120.pdf
[ii] Medicare Payment Advisory Commission. (2023, June 15). Report to the Congress: Medicare and the Health Care Delivery System. https://www.medpac.gov/wp-content/uploads/2023/06/Jun23_MedPAC_Report_To_Congress_SEC.pdf
[iii] Ibid.
[iv] American Hospital Association. (2023, September). Medicare Site-neutral Legislative Proposals Under Consideration Would Jeopardize Access to Care for Patients and Communities. https://www.aha.org/fact-sheets/2023-09-05-medicare-site-neutral-legislative-proposals-under-consideration-would-jeopardize-access-care-patients.
[v] Ibid.
[vi] Ibid.